When I tell people that living with pancreatic cancer has some blessings, my statement typically is met with a curious disbelief that leaves me uncomfortable for having said it. But, the blessings are oddly true. Each day feels more alive, intense and important. I take the opportunity to tell my family and friends what they mean to me in great detail and with great regularity. It creates a life of love.
Meeting brilliant, courageous scientists and doctors (including my doctors, William Isacoff and Allyson Ocean) committed to changing the course of this disease is among these blessings as well. Knowing them helps me deal with the incomprehensible truth that there are no long-term treatments, no early detection tests and no cures for this most lethal cancer.
It may be unusual to call scientists courageous but research challenges in pancreatic cancer are immense. Pancreas tumors are complex and continually mutating. The K-RAS gene found to be mutated in the majority of pancreatic cancer patients has continued to
stymie researchers' efforts to block it. The stroma, the barrier surrounding the pancreatic tumor, is a resistant shield preventing therapy from reaching the tumor effectively.
Although the past 40 years have given us very few (and no long-term) treatments for pancreatic cancer, there is now new progress from a number of exceptional scientists willing to focus on these challenges.
Getting to know some of these amazing scientists has not only enhanced my life, but it has reinforced the fact that pancreatic cancer patients and families must keep informed of the best science efforts. It is the key to extending our lives.
These organizations can provide some information. The
Lustgarten Foundation is the nation's largest private funder of pancreatic cancer research; 100 percent of its funding goes to research due to the support of Cablevision. The
Pancreatic Cancer Action Network is another valuable source for science and patient information.
Dr. Isacoff introduced me to
Dr. David Tuveson, the director of research at The Lustgarten Foundation and director of The Lustgarten Pancreatic Cancer Research Laboratory in partnership with Cold Spring Harbor Laboratory. This is a picture of Dr. Tuveson.
When my family and I went to see the lab we were so galvanized. The scientific attack on pancreatic cancer made us feel that we were seeing history happen, giving us a fortifying glimpse into a positive future.
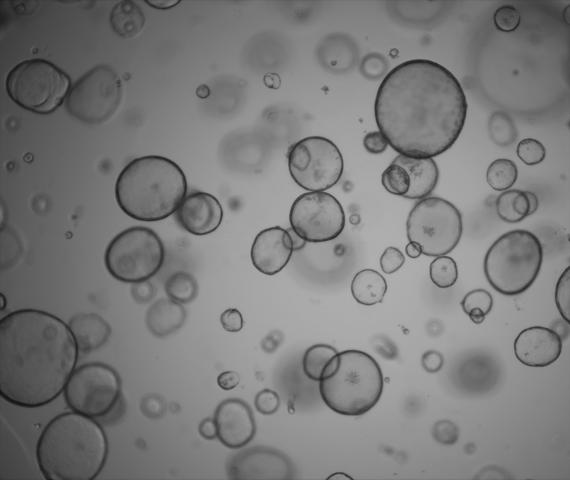
One of the projects of the lab is the generation of organoids, a new breakthrough investigative mechanism for pancreatic cancer. What makes organoids so exciting is that they can reproduce pancreatic tissue samples giving patients many potential benefits. This is a picture of the organoid from the lab.
Here is the paper in
Cell.
First, these living tumor cells can be tested over time with a wide range of medications, enabling scientists to find biomarkers and identify new combinations of drugs to treat the disease. Simply, in the future, instead of pancreatic cancer patients being tested with new medications, organoids can endure that experience.
Second, organoids can speed up research and the search for treatment options which we urgently need. As Dr. Tuveson noted, "Patients are dying. Organoids will speed up the process for creating robust clinical trials by providing a whole new set of data based on this new access to living tumor tissue."
Third, organoids create more tissue for testing. A major research constraint has been the lack of tissue. Organoids will create a supply in pancreatic cancer tissue that will assist investigators. Indeed the lab provides an "organoid training school" so that many institutions will have access to the technology and tissue.
A young scientist, Dr. Hervé Tiriac, a postdoctoral fellow at the lab, has the responsibility to ensure that more than 40 organoids under his care are growing well and are being tested. Here is a picture of Dr. Tiriac.
Hervé's deep intelligence and passion for his work are clearly evident. He told me that he found this passion for making a difference in pancreatic cancer in a round-about way. A graduate of the University of California at Davis and San Diego, he first focused on hardcore genetics and biochemistry.
While in graduate school, he met Dannielle Engle a fellow scientist, and that changed his life. Her father had died of pancreatic cancer and her professional and personal mission is to cure the disease. Hervé and Dannie, now married, are a dynamic force for progress, working together in the lab.
I learned a lot talking to Hervé about the potential of organoids to extend life spans. Along with the organoid tumor cells, he is also growing organoids with normal cells. He said, "The hope is to weed out novel therapeutics that would be too toxic. That's why we test normal cells too."
He explained that organoids could help address the differences within pancreatic cancer by breaking tumors into subclasses that would be treated by different therapeutics. "With more tissue you have more to learn." he said. "Organoids can eventually offer models of personalized medicine for patients and become an excellent way to analyze the link between genetic mutations and treatment."
Talking to Hervé made me realize that organoid research may lead to the better design of clinical trials and faster, more effective treatment.
Staying on top of what is happening in leading scientific research is a lifeline for all pancreatic cancer patients and families. We have the most lethal cancer, and yet only 2 percent of the
federal funding is directed to pancreatic cancer research!
While many extraordinary scientists are now working for cures and early detection tests, more than
40,000 people this year will die of pancreatic cancer.
We must all be familiar with the science and support these scientists. And we must advocate urgently for more private and public research funding. It will save our lives.
This blog is dedicated to Jeff Schmahl, my friend on this path, who inspired so many with his wonderful life.
 Pancreatic cancer is a formidable foe. It grows fast and spreads quickly, often before any symptoms appear. And because of its notorious resistance to treatment, 97 percent of patients aren't alive five years after diagnosis.
Pancreatic cancer is a formidable foe. It grows fast and spreads quickly, often before any symptoms appear. And because of its notorious resistance to treatment, 97 percent of patients aren't alive five years after diagnosis.








 Our program is managed by
Our program is managed by