Tumor cells associated with pancreatic cancer often behave like communities by working with each other to increase tumor spread and growth to different organs. Groups of these cancer cells are better than single cancer cells in driving tumor spread, according to new research from the Perelman School of Medicine at the University of Pennsylvania published in Cancer Discovery online in advance of the print issue.
Ben Stanger, MD, PhD, a professor in the division of Gastroenterology, and first author Ravi Maddipati , MD, an instructor in the division of Gastroenterology, say that these results may prove useful in designing better targeted therapies to stop tumor progression and provide an improved non-invasive method for detecting early disease states in this highly lethal cancer. Stanger is also a professor in the department of Cell and Developmental Biology and the Abramson Family Cancer Research Institute.
Cancer genome studies have shown that within most tumors there exists many different types of cells, which often harbor unique genetic alterations that lead to differences in their physiological properties. Previous studies using tumor cells lines suggested that these different tumor cell types may interact with each other to produce a more aggressive type of cancer. However, the mechanisms by which tumor cells interact to enhance the spread of cancer remained unclear.
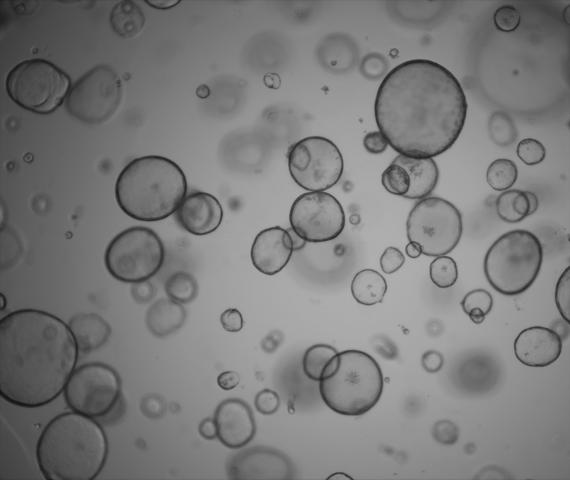
From other earlier studies, the Penn team also knew that cells from a primary tumor do better replicating and surviving in a group rather than if they are grown on their own. From this, the researchers asked if the spread of cancer is primarily derived from one cell or a cell cluster derived from the interactions between different cancer cell types. Stanger and Maddipati tested the hunch that clusters of cells of different genetic makeup were better at establishing secondary tumors and found that a significant fraction of metastases involve seeding by more than one type of tumor cell during the natural course of pancreatic tumor progression.
To understand this spread, the Penn researchers developed a mouse model that uses multiple fluorescent proteins to tag and track different pancreatic cancer cells as they enter the bloodstream and spread to distant organs. In this mouse model, mutations in Kras and p53 genes resulted in the formation of individual tumor cell populations that were labeled with different colors. Similar to humans, the mice developed tumors at secondary sites including the liver, lung, peritoneum, and diaphragm. They observed that these metastases were often made of cells from at least two different colors of tumor cell populations. To understand how these multi-colored lesions originated they examined blood from these mice and found that tumor cells in circulation frequently occurred as clusters comprised of different colored cancer cells.
What's more, they also found that once these multi-colored clusters arrived at the secondary sites, the exact characteristics of subsequent growth was heavily dependent on the organ in which they now resided. During cell expansion in the peritoneum and diaphragm the lesions remained multi-colored, whereas in the lung and liver only a single color population was able to grow out. This suggested that specific factors in each organ may also influence the evolution of metastases.
"These results provide an unprecedented window into the cellular dynamics of tumor evolution and suggest that interactions between subpopulations of tumor cell types contribute to metastatic progression from initial tumors," Stanger said. "The finding that metastases are frequently polyclonal and that subsequent cellular behavior is site-dependent also gives us insight into the origins and evolution of clonal diversity in metastatic disease."
"If cells do cooperate during metastasis, what is the molecular basis for their communication, and can we hit that?," Stanger asked. The work also reinforces the importance of finding tumor cell clusters in the blood as a mechanism of detecting cancer metastasis earlier.
Source:
Penn Medicine